I remember the day I opened my patient experience scores for the first time.
I was a surgeon, confident in my training, deeply committed to my patients, and convinced I was doing everything right. So, when I saw my overall score placed me in the 5th percentile nationwide, I was stunned. Fifth percentile. Not 50th. Fifth. I sat in silence, blinking at the screen. Then I cried—for a week.
How could this be? Didn’t my patients know how much I cared? Didn’t they see the sleepless nights I spent poring over their labs, worrying over their scans, replaying every decision in my head? How could I pour so much of myself into their care and be rated so poorly?
Like many physicians, I had plenty of rationalizations. Small sample size. Language barriers. Maybe they were rating the clinic parking, or their wait time, not me. Maybe they had received difficult news. Maybe they just didn’t respond if they were happy. And maybe—just maybe—these scores didn’t really reflect the quality of care.
But beneath all that noise, a quieter question lingered: What if they were right?
What if, despite my best intentions, I wasn’t truly connecting? What if I had become so efficient, so focused on fixing, that I’d stopped seeing the human sitting across from me?
Once I moved past the shame, I got curious. I asked a hospital social worker to shadow my clinic visits. I invited non-clinical staff to sit in and offer their perspective. Then I partnered with a colleague trained in communication to review the feedback and dissect the scores. He helped me see what I couldn’t: how often I jumped straight to diagnosis before listening to the patient’s real concern. How rarely I asked if they felt heard. How even subtle cues—eye contact, body language, pauses—could build or erode trust in a matter of seconds.
I began making changes. Small at first: greeting patients by name, sitting down instead of standing, asking one more question before I spoke. I learned to slow down just enough to see the person before me.
The results didn’t come overnight. My scores rose, but slowly. I still got the occasional harsh comment. But I stayed the course. I took a course on medical communication. I read books. I shadowed top-performing physicians in the 95th percentile and watched how they listened, how they smiled, how they made patients feel safe.
Eventually, my own scores climbed. I was no longer the outlier—I was the leader.
And then, I became the teacher.
I was asked to help elevate the scores of our entire physician group. So I started with what I knew: humility. I met with each provider privately. I showed them their scores, then gave them time to process. I listened to their skepticism, their frustration, their fear. Then, I offered tools, just as someone once had for me. Over time, as confidence grew, we made the scores visible across the group. Some friendly competition emerged. Best of all, the conversations changed—from “this isn’t fair” to “how can I do better?”
Today, I look forward to my scores. I read every comment. I take the negative ones seriously, but not personally. When something stings, I debrief with trusted peers, gather context, and reflect on what I can learn.
Patient experience is now a cornerstone of how I practice medicine. My patients still receive the same evidence-based, expert care—but now, they also feel seen. Heard. Respected.
The truth is, I didn’t become a better doctor by learning new procedures or memorizing new guidelines. I became a better doctor by remembering I was a human first.
The moral of the story?
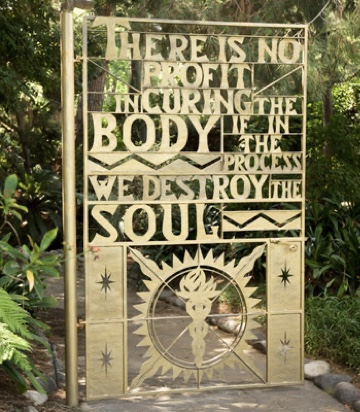
Clinical excellence and human connection are not mutually exclusive. In fact, they are inseparable. Patients will rarely remember every detail of their diagnosis—but they will always remember how you made them feel.
And when you can bring both skill and compassion into the room, healing begins in more ways than one.
Leave a comment